BJS Academy>Continuing surgical ...>Biomarkers for pancr...
Surgical digest
Biomarkers for pancreatic cancer: going beyond the impossible?
Daniel Ansari
Department of Surgery, Clinical Sciences Lund, Lund University and Skåne University Hospital, Lund Sweden
Roland Andersson
Department of Surgery, Clinical Sciences Lund, Lund University and Skåne University Hospital, Lund Sweden
Related articles
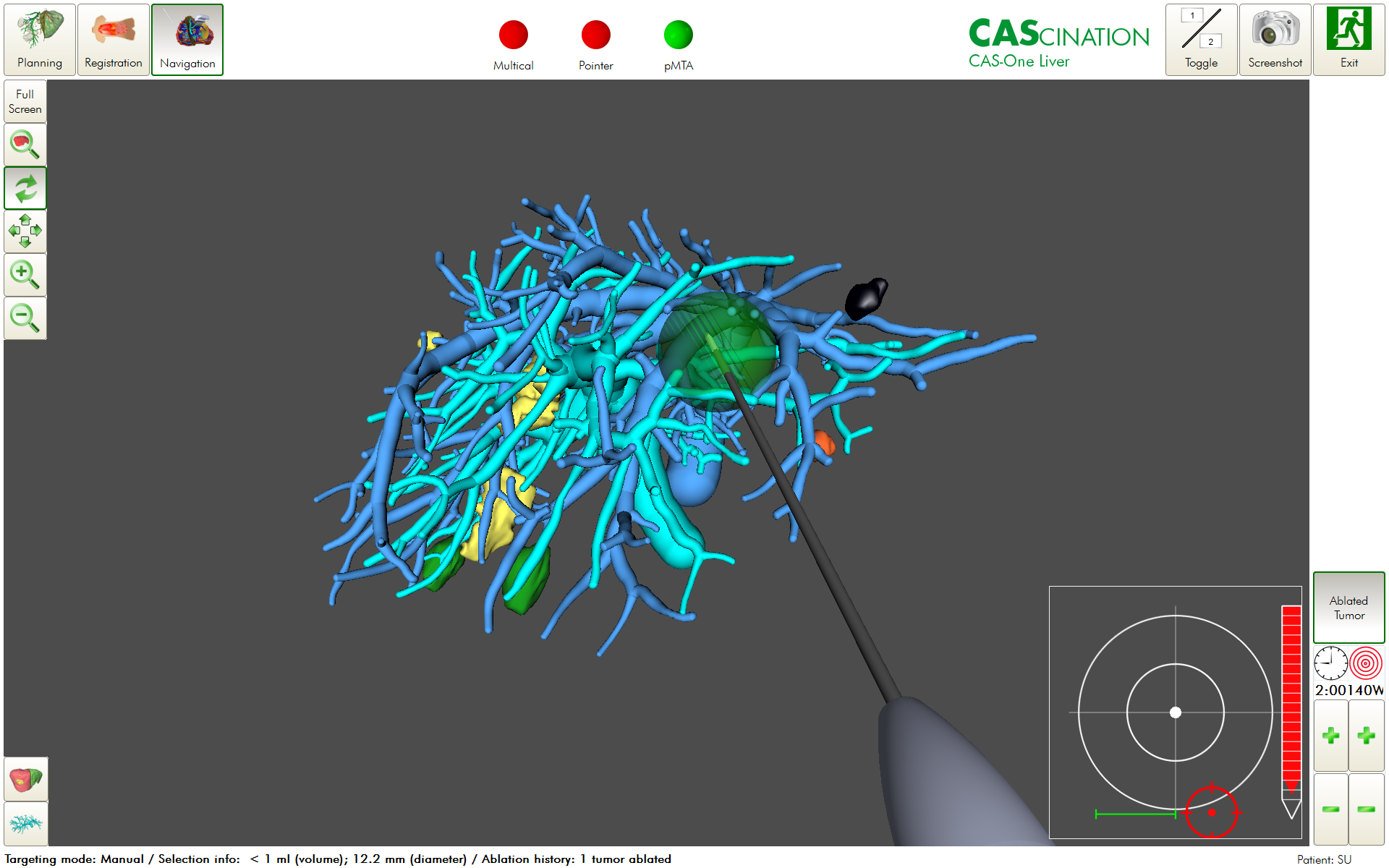
Image-guided ablation for liver tumours – an addition to the armamentarium of multidisciplinary oncological and surgical approaches
Petter Frühling MD, PhD, Barbara Seeliger, MD, PhD, Ana Karla Uribe Rivera, MD, Jacob Freedman, MD, PhD, Mariano Giménez, MD, PhD
The treatment of primary and metastatic liver tumours by ablation is not new. Advances in guidance systems, image fusion and new concepts of 3D tumour localisation and treatment, together with the current concepts of computer-assisted surgery that augment the senses (image-guided surgery), cognition (artificial intelligence), and execution (robotics), have enabled a fundamental change in the concept of ablation and have shaped image-guided ablation, also called precision ablation or Ablation 2.01. These changes have improved accuracy and in many cases made the oncological outcomes of ablation equal to those of surgical resection. Indications for ablation therapies in liver tumours Treatment options for colorectal liver metastases (CRLM) and hepatocellular carcinoma (HCC) include a combination of surgery, local ablation, and chemotherapy. For HCC, ablation is part of the treatment guidelines, such as the Barcelona Clinic Liver Cancer (BCLC) classification2, 3 and the ESMO (European Society for Medical Oncology) clinical practice guidelines4. It is used for smaller tumours and in patients with advanced cirrhosis, where resection may be more difficult3, 5. Liver resection is considered the gold standard for CRLM6-8. Recently, however, the COLLISION Trial Group presented a treatment algorithm for patients with CRLM without extrahepatic disease, recommending ablation for deeply situated metastases and unresectable metastases smaller than 3 cm7.

2024 ASGBI BJS Prize: Tumour targeted oxygen-generating nanoparticles for enhanced radiotherapy in the treatment of pancreatic cancer
Sian Farrell presents her BJS Prize winning lecture “Tumour targeted oxygen-generating nanoparticles for enhanced radiotherapy in the treatment of pancreatic cancer” from the 2024 Association of Surgeons of Great Britain and Ireland (ASGBI) International Surgical Congress.
Can recurrent diverticulitis be predicted?
Lucia Sobrinoa, Marta Climent, Clara Santanach, Sebastiano Biondo
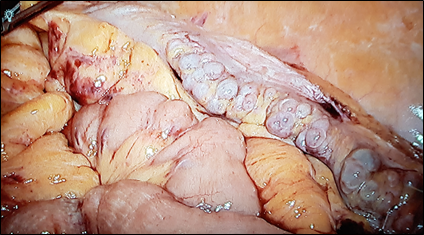
Diverticular disease is a common disorder, and recent guidelines report on new treatment strategies such as non-antibiotic management. Patients with diverticular disease are increasingly being treated as outpatients. In addition, fewer patients are undergoing emergency surgery whereas there is an increase in the use of elective and laparoscopic surgery in the management of diverticulitis. However, several aspects are still controversial. Strong evidence still lacks for the therapeutic management of patients with recurrent episodes of acute diverticulitis or patients with persistent abdominal symptoms after acute attacks. The European Society of Coloproctology (ESCP) guideline committee reviewed the literature and developed the European guidelines for the management of diverticular disease of the colon in 2020. In spite of the existence of several different classifications for diverticulitis, the committee decided neither to create another classification nor to endorse any of the existing ones. Nevertheless, phlegmonous diverticulitis, considered as uncomplicated by most of the classifications, is a matter of concern since it includes about 70% of the patients with acute diverticulitis. This group of patients may be clinically heterogeneous in terms of characteristics or disease evolution, which in some cases might be complicated. Patients at risk that belong to initially uncomplicated stage need to be identified in order to prevent complications and receive the most appropriate medical/surgical treatment. Classically, colonic resection after the second episode of acute diverticulitis has been supported, since any following episodes will respond insufficiently to medical treatment and with higher morbidity and mortality2. Recently, it was reported that 6.8-27.7%3,4 of patients with acute diverticulitis treated conservatively may require surgical intervention due to complicated diverticulitis or persistent symptoms, most of them during the first year of follow-up. In addition, elective sigmoidectomy seems to be related with a better quality of life (QOL) compared with conservative management in patients with recurring diverticulitis and/or ongoing complaints5,6. Nowadays, the main reason to perform elective sigmoid colectomy (Fig 1) in patients with recurrent disease or with ongoing symptoms after an acute episode of diverticulitis is to improve their QOL. In fact, there are many patients in whom initial antibiotic treatment fails, leading to sub-acute / chronic diverticulitis. In these patients the differentiation between sub-acute ongoing diverticulitis which never resolved, i.e. persisting disease, and a true recurrence is very difficult7. Chronic diverticulitis (Fig 1), considered as a true condition for the first time by the ESCP group, occurs when there is colonic wall thickening or chronic inflammation of the mucosa1. It can appear when an acute diverticulitis does not resolve completely, and it can have an important impact on QOL of the patients, causing persistent abdominal symptoms (abdominal pain, bloating) and changes in bowel habit. However, the uncertainty of the evolution of the disease and the lack of clear signs to identify which patients will develop a chronic condition, make the selection of patients and the best moment to advise surgical resection difficult. Colonic resection has been shown to effectively reduce the number of recurrences, but it should be kept in mind that it is a major surgery with potential severe complications1. The distinction between Irritable Bowel Syndrome (IBS) and symptoms related to chronic diverticulitis after an episode of diverticulitis is of utmost importance, because IBS is a functional disorder and should not be treated surgically8. Endoscopy could help in those cases where differential diagnosis is difficult5. It should be noted that after sigmoidectomy, 25% of patients persist with functional symptoms and abdominal pain9.
Copied!
Connect

Copyright © 2025 River Valley Technologies Limited. All rights reserved.








.jpg)



