BJS Academy>Cutting edge blog>Re evaluating enoxap...
Re-evaluating enoxaparin for thromboprophylaxis in liver transplantation: a closer look
Dipesh Kumar Yadav, MD, PhD
Department of General Surgery, The Third Clinical Institute Affiliated to Wenzhou Medical University, Wenzhou People's Hospital
Yiren Hu, MD, PhD
Department of General Surgery, The Third Clinical Institute Affiliated to Wenzhou Medical University, Wenzhou People's Hospital
Related articles

Team design as innovation in perioperative care: the case of HPB anesthesiology
Julie Hallet, MD MSC, Naheed Jivraj, MD MSc
Change takes time – in all fields, including surgery. Yet, innovation is highly prized. The latest tools and technologies are celebrated and heavily invested in. But not all improvements require new technology.
For example, robotic pancreatic surgery is being adopted worldwide at a cost of millions in capital investment and ongoing expenses. Evidence shows it is mostly non-inferior to the standard of care.1–4 Another example is histotripsy for liver tumors, which has been rapidly purchased across multiple centers since FDA approval in 2023, spreading like mushrooms after the rain. Evidence is limited to technical feasibility, with no proof of superiority over standard care.5 Both technologies are used only in selected patients. By contrast, high-volume anesthesiology care for hepato-pancreato-biliary (HPB) surgery is associated with15% lower odds of 90-day major morbidity (OR 0.85, 95% CI 0.76–0.94), requires no capital investment, no recurring costs, and applies to all patients.
We are not debating or questioning the benefits of these technologies or the need to invest in new treatments. Rather, we would like to ask: if we are so willing to spend vast sums on new technology, why are we far less inclined to redesign how operative teams are organized?
Guest blog: Venous resection during pancreatoduodenectomy – there is still much to gain
J.V. Groen, Department of Surgery, Leiden University Medical Centre, Leiden, J.V.Groen@lumc.nl N. Michiels, Department of Surgery, Leiden University Medical Centre, Leiden, N.Michiels@lumc.nl J.S.D. Mieog, Department of Surgery, Leiden University Medical Centre, Leiden, J.S.D.Mieog@lumc.nl
IMPORTANCE
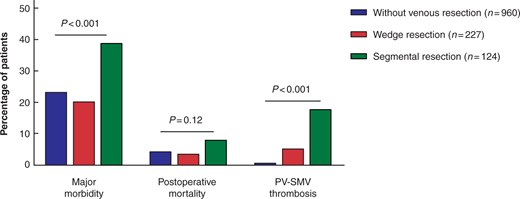
The use of venous resection (portal or superior mesenteric vein [PV-SMV]) during pancreatoduodenectomy is increasing.1-4 In a recent international survey, we found that most pancreatic surgeons prefer a segmental resection with primary anastomosis over a partial wedge resection, because of a lower perceived risk of complications.5 The impact of the type of venous resection (wedge or segmental) on postoperative morbidity and survival is poorly understood in current literature.
QUESTION
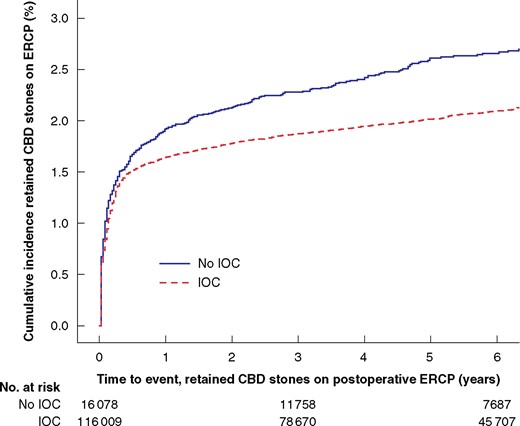
Video: Intervention versus surveillance in patients with common bile duct stones detected by intraoperative cholangiography
Each year 13 000 patients undergo cholecystectomy in Sweden, and routine intraoperative cholangiography (IOC) is recommended to minimize bile duct injuries. IOC plus an intervention to remove CBD stones identified during cholecystectomy was associated with reduced risk for retained stones and unplanned ERCP, even for the smallest asymptomatic CBD stones in this BJS study.
Copied!
Connect

Copyright © 2026 River Valley Technologies Limited. All rights reserved.



.png)





.jpg)



