BJS Academy>Cutting edge blog>Guest blog: Venous r...
Guest blog: Venous resection during pancreatoduodenectomy – there is still much to gain
J.V. Groen, Department of Surgery, Leiden University Medical Centre, Leiden, J.V.Groen@lumc.nl N. Michiels, Department of Surgery, Leiden University Medical Centre, Leiden, N.Michiels@lumc.nl J.S.D. Mieog, Department of Surgery, Leiden University Medical Centre, Leiden, J.S.D.Mieog@lumc.nl
3 December 2021
Guest Blog HPB
Related articles
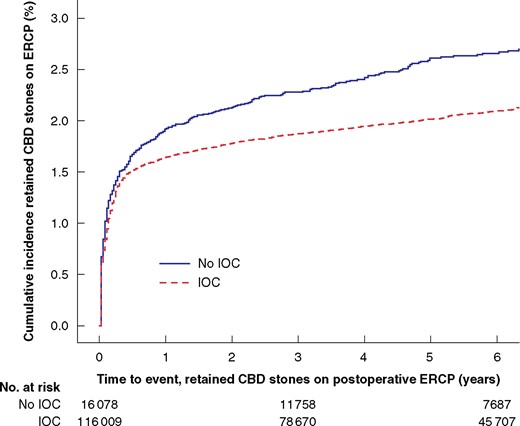
Video: Intervention versus surveillance in patients with common bile duct stones detected by intraoperative cholangiography
Each year 13 000 patients undergo cholecystectomy in Sweden, and routine intraoperative cholangiography (IOC) is recommended to minimize bile duct injuries. IOC plus an intervention to remove CBD stones identified during cholecystectomy was associated with reduced risk for retained stones and unplanned ERCP, even for the smallest asymptomatic CBD stones in this BJS study.
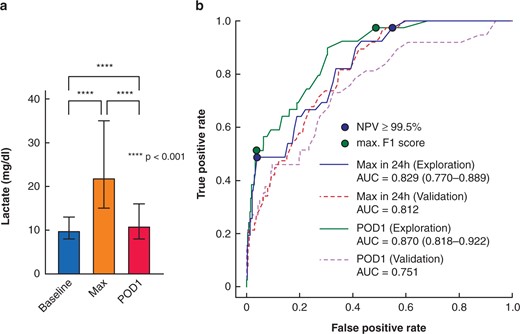
Video: Early postoperative arterial lactate concentrations to stratify risk of post-hepatectomy liver failure
Post-hepatectomy liver failure (PHLF) represents the major determinant for death after liver resection. Early recognition is essential. Early postoperative lactate values are powerful, readily available markers for clinically relevant PHLF and associated complications after hepatectomy with potential for guiding postoperative care. This video explains the recent study published in BJS.

Guest blog: Death following pulmonary complications of surgery before and during the SARS-CoV-2 pandemic: how to compare apples and oranges?
Kenneth A McLean, Sivesh K Kamarajah, James C Glasbey
Early in the pandemic, it was recognised that patients had a higher rate of death associated with pulmonary complications if they become infected with SARS-CoV-2 in the perioperative period 1. However, the key question is why? Was this solely down to SARS-CoV-2 infections, was this due to differences in who was prioritised for surgery, or due to some other reason? These are difficult questions to answer, especially without comparable data from the pre-pandemic period.
To address this, our paper published in the BJS pools together two large-scale, prospective and multi-specialty international cohorts 2: one from the pre-pandemic period from the STARSurg Collaborative 3 and another from during the pandemic from the COVIDSurg collaborative 4. Since these projects both included elective abdominal cancer surgery patients, and collected similar data on them and their postoperative outcomes, we were able to make a fair comparison between these cohorts.
Overall, there was only a minority of patients with a perioperative SARS-COV-2 infection (4.3%), which is reassuring that most patientsundergoing surgery during this period were safeguarded. Interestingly, when postoperative outcomes were compared between the periods, the pulmonary complication rate observed was relatively similar (7.1% [before] vs 6.3% [during], p=0.158) but the 30-day mortality was much higher (0.7% [before] versus 2.0% [during], p<0.001). This was perhaps due to more “severe” pulmonary complications during the pandemic, e.g. a higher proportion of patients with acute respiratory distress syndrome.
Copied!
