BJS Academy>Cutting edge blog>Completion pancreate...
Completion pancreatectomy or a pancreas-preserving procedure during relaparotomy for pancreatic fistula after pancreatoduodenectomy: a multicentre cohort study and meta-analysis.
J.V. Groen, Department of Surgery, Leiden University Medical Centre, Leiden, J.V.Groen@lumc.nl
J.S.D. Mieog, Department of Surgery, Leiden University Medical Centre, Leiden, J.S.D.Mieog@lumc.nl
19 December 2022
Guest Blog HPB
Related articles
Guest blog: Venous resection during pancreatoduodenectomy – there is still much to gain
J.V. Groen, Department of Surgery, Leiden University Medical Centre, Leiden, J.V.Groen@lumc.nl N. Michiels, Department of Surgery, Leiden University Medical Centre, Leiden, N.Michiels@lumc.nl J.S.D. Mieog, Department of Surgery, Leiden University Medical Centre, Leiden, J.S.D.Mieog@lumc.nl
IMPORTANCE
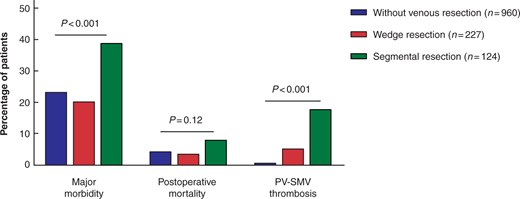
The use of venous resection (portal or superior mesenteric vein [PV-SMV]) during pancreatoduodenectomy is increasing.1-4 In a recent international survey, we found that most pancreatic surgeons prefer a segmental resection with primary anastomosis over a partial wedge resection, because of a lower perceived risk of complications.5 The impact of the type of venous resection (wedge or segmental) on postoperative morbidity and survival is poorly understood in current literature.
QUESTION
Video: Intervention versus surveillance in patients with common bile duct stones detected by intraoperative cholangiography
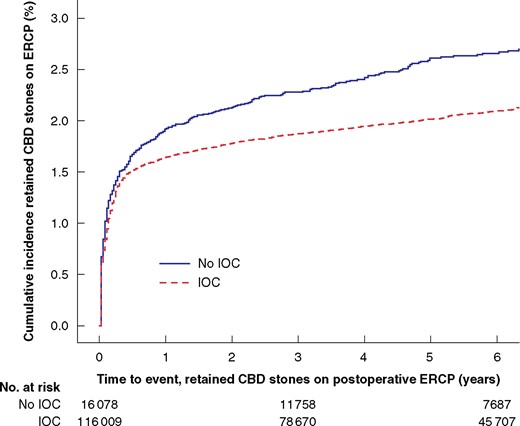
Each year 13 000 patients undergo cholecystectomy in Sweden, and routine intraoperative cholangiography (IOC) is recommended to minimize bile duct injuries. IOC plus an intervention to remove CBD stones identified during cholecystectomy was associated with reduced risk for retained stones and unplanned ERCP, even for the smallest asymptomatic CBD stones in this BJS study.
Video: Early postoperative arterial lactate concentrations to stratify risk of post-hepatectomy liver failure
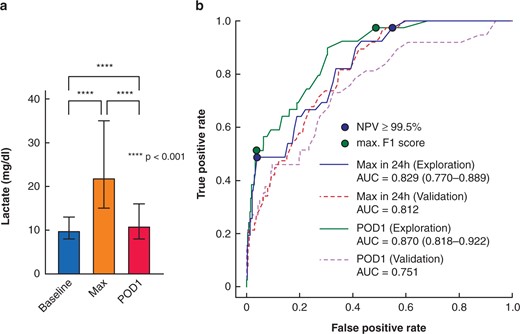
Post-hepatectomy liver failure (PHLF) represents the major determinant for death after liver resection. Early recognition is essential. Early postoperative lactate values are powerful, readily available markers for clinically relevant PHLF and associated complications after hepatectomy with potential for guiding postoperative care. This video explains the recent study published in BJS.
Copied!
Connect

Copyright © 2026 River Valley Technologies Limited. All rights reserved.



.png)





.jpg)



