BJS Academy>Continuing surgical ...>The management of oe...
(1)
Surgical digest
The management of oesophageal cancer: the surgeon’s perspective
Eider Talavera-Urquijo, MD PhD
Department of Surgery University Hospital of Donostia Donostia-San Sebastián Spain
Bas P. L. Wijnhoven, MD PhD
Department of Surgery Erasmus University Medical Centre Rotterdam Rotterdam The Netherlands
Related articles
The evolution of surgical treatment for achalasia: from experimental evidence to real-world impact
Luigi Marano, MD, PhD, Natale Di Martino, MD
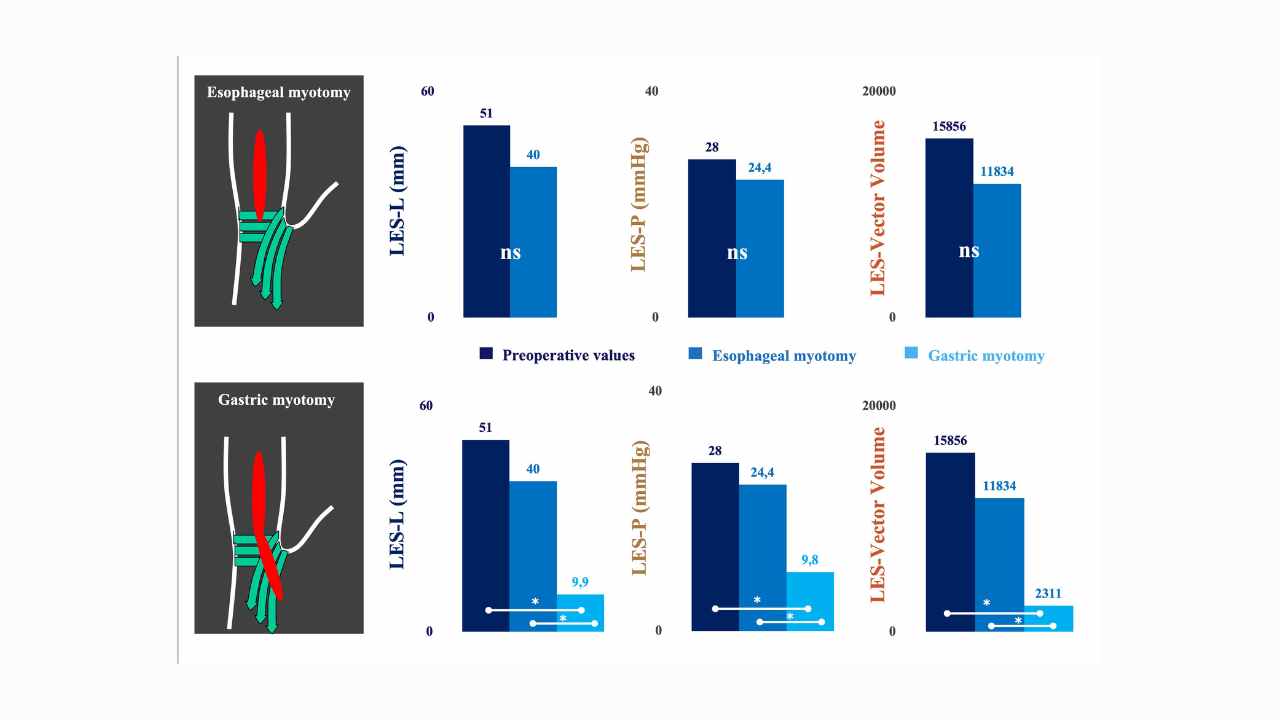
The optimal length of myotomy Achalasia, an immune-mediated disorder of oesophageal dysmotility, is characterized by impaired relaxation at the oesophagogastric junction (OGJ) and the absence of peristalsis upon swallowing1. These pathological alterations culminate in a functional outflow obstruction at the OGJ, leading to inefficient transit of the food bolus and manifesting as symptoms of dysphagia and non-acid regurgitation2. Therapeutic interventions aim to disrupt the OGJ complex to facilitate passive bolus transit into the stomach, thereby alleviating symptoms and improving long-term quality of life. The primary objective of current therapeutic options is to achieve sustained relief of dysphagia while minimizing the risk of symptom recurrence. Standard treatments such as pneumatic dilation, laparoscopic Heller myotomy (LHM), and per-oral endoscopic myotomy (POEM) are employed to lower oesophageal sphincter (LOS) pressure, thereby enhancing oesophageal outflow dynamics and ameliorating symptoms3–5. These interventions represent frontline approaches in the management of achalasia, providing effective palliation by addressing the underlying pathophysiology of the condition. The surgical management of achalasia stands out as the most effective approach among available treatments, offering favourable short- and long-term clinical outcomes5,6,7. This efficacy is particularly pronounced with the adoption of minimally invasive techniques, which have now become the preferred treatment for patients with idiopathic achalasia. However, despite the advantages of laparoscopic myotomy, it is important to acknowledge inherent limitations associated with the laparoscopic approach, such as bi-dimensional vision and restricted range of movement, which may impact on surgical precision. Recently, robotic technology has emerged as a promising alternative, with proponents suggesting its potential to reduce intraoperative oesophageal perforation rates and improve postoperative quality of life following Heller myotomy8. This potential enhancement is primarily attributed to the three-dimensional visualization and enhanced surgical dexterity offered by robotic systems.
Can recurrent diverticulitis be predicted?
Lucia Sobrinoa, Marta Climent, Clara Santanach, Sebastiano Biondo
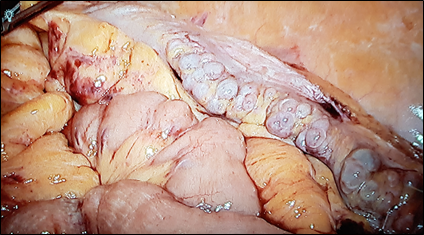
Diverticular disease is a common disorder, and recent guidelines report on new treatment strategies such as non-antibiotic management. Patients with diverticular disease are increasingly being treated as outpatients. In addition, fewer patients are undergoing emergency surgery whereas there is an increase in the use of elective and laparoscopic surgery in the management of diverticulitis. However, several aspects are still controversial. Strong evidence still lacks for the therapeutic management of patients with recurrent episodes of acute diverticulitis or patients with persistent abdominal symptoms after acute attacks. The European Society of Coloproctology (ESCP) guideline committee reviewed the literature and developed the European guidelines for the management of diverticular disease of the colon in 2020. In spite of the existence of several different classifications for diverticulitis, the committee decided neither to create another classification nor to endorse any of the existing ones. Nevertheless, phlegmonous diverticulitis, considered as uncomplicated by most of the classifications, is a matter of concern since it includes about 70% of the patients with acute diverticulitis. This group of patients may be clinically heterogeneous in terms of characteristics or disease evolution, which in some cases might be complicated. Patients at risk that belong to initially uncomplicated stage need to be identified in order to prevent complications and receive the most appropriate medical/surgical treatment. Classically, colonic resection after the second episode of acute diverticulitis has been supported, since any following episodes will respond insufficiently to medical treatment and with higher morbidity and mortality2. Recently, it was reported that 6.8-27.7%3,4 of patients with acute diverticulitis treated conservatively may require surgical intervention due to complicated diverticulitis or persistent symptoms, most of them during the first year of follow-up. In addition, elective sigmoidectomy seems to be related with a better quality of life (QOL) compared with conservative management in patients with recurring diverticulitis and/or ongoing complaints5,6. Nowadays, the main reason to perform elective sigmoid colectomy (Fig 1) in patients with recurrent disease or with ongoing symptoms after an acute episode of diverticulitis is to improve their QOL. In fact, there are many patients in whom initial antibiotic treatment fails, leading to sub-acute / chronic diverticulitis. In these patients the differentiation between sub-acute ongoing diverticulitis which never resolved, i.e. persisting disease, and a true recurrence is very difficult7. Chronic diverticulitis (Fig 1), considered as a true condition for the first time by the ESCP group, occurs when there is colonic wall thickening or chronic inflammation of the mucosa1. It can appear when an acute diverticulitis does not resolve completely, and it can have an important impact on QOL of the patients, causing persistent abdominal symptoms (abdominal pain, bloating) and changes in bowel habit. However, the uncertainty of the evolution of the disease and the lack of clear signs to identify which patients will develop a chronic condition, make the selection of patients and the best moment to advise surgical resection difficult. Colonic resection has been shown to effectively reduce the number of recurrences, but it should be kept in mind that it is a major surgery with potential severe complications1. The distinction between Irritable Bowel Syndrome (IBS) and symptoms related to chronic diverticulitis after an episode of diverticulitis is of utmost importance, because IBS is a functional disorder and should not be treated surgically8. Endoscopy could help in those cases where differential diagnosis is difficult5. It should be noted that after sigmoidectomy, 25% of patients persist with functional symptoms and abdominal pain9.
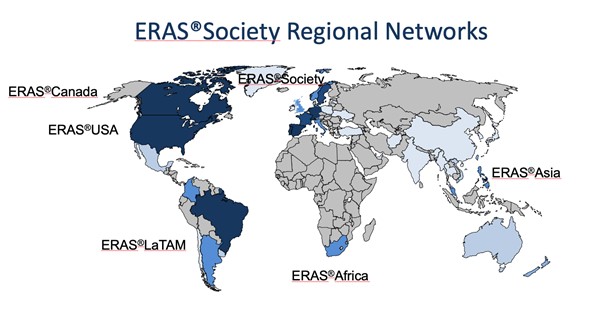
ERAS – yesterday, today and also for tomorrow? The ERAS Society perspective.
Olle Ljungqvist, Ulf Gustafsson, Hans D. de Boer
ERAS so far It is more than 25 years ago that a multimodal approach to recovery after major surgery, called fast track surgery, was first proposed1,2. Combined with laparoscopic surgery it showed that old and frail patients were fit to leave the hospital in two days after major surgery3. Larger follow up studies reported that this could be achieved with fast track surgery alone. This inspired a group of surgeons from Northern Europe to form the Enhanced Recovery After Surgery (ERAS) Study Group in 20014. The members hypothesized that bringing together all potential stress reducing and recovery improving care elements into one program, would enhance recovery after surgery. The first ERAS protocol was published in 20055. But alongside the guideline there was a need to also organize care in a new way to make ERAS fully functioning6 (Table 1). When the guideline was tested a clear relationship was shown with more care elements in the protocol in use and improved outcomes regarding both complications, length of stay and readmissions suggesting that detailed audit would be key7-9.
Copied!
