BJS Academy>Continuing surgical ...>Defining the role fo...
Surgical digest
Defining the role for robotics in endocrine surgery – benefits and challenges
Jason Ramsingh
Consultant General and Endocrine Surgeon Royal Victoria Infirmary Newcastle
Related articles
Thyroidectomy for Graves’ disease
Martin Almquist, Frédéric Triponez, Carolyn D. Seib
Graves’ disease (GD) is an autoimmune disease in which thyroid receptor stimulating antibodies cause the thyroid to overproduce thyroid hormone, leading to hyperthyroidism. Untreated hyperthyroidism can lead to adverse clinical outcomes, including severe hypertension, cardiac arrhythmias and death. Graves’ disease is named after the Irish surgeon Robert James Graves, who was the first to identify the hallmark clinical features of GD, which include symptoms of hyperthyroidism associated with a diffuse goitre, thyroid eye disease, and pretibial myxoedema. Public figures with GD include the British Comedian Marty Feldman, singer-songwriter Missy Elliott, former U.S. president George H.W. Bush and his wife, former first lady Barbara Bush. Marty Feldman, Missy Elliot, and Barbara Bush all had thyroid eye disease or Graves’ ophthalmopathy, which occurs in up to 25% of patients with GD.1,2 Graves’ ophthalmopathy is caused by autoantibody stimulation of orbital fibroblasts and adipocytes, which leads to inflammation due to cell proliferation and the local accumulation of glycosaminoglycans.3 Guidelines by the European Thyroid Association (ETA), the American Thyroid Association (ATA) and the American Association of Endocrine Surgeons (AAES) state that antithyroid drugs , radioiodine ablation (RAI), and thyroidectomy are treatment options for GD.4-6 The administration of drugs, most commonly methimazole, results in remission in approximately 50% of patients with GD, but is associated with adverse events including pruritic rash, agranulocytosis, and hepatotoxicity.7, 8 Given the majority of adverse events occur early in the medical treatment of GD, long-term treatment is safe and may lead to higher rates of remission.9,10 The ETA and ATA recommend total thyroidectomy for GD with ophthalmopathy, large goitres, co-existing primary hyperparathyroidism, suspected or proven thyroid cancer, and current or planned pregnancy.4,5. Relative contraindications include significant patient comorbidity and/or limited life expectancy, prior neck surgery and/or irradiation.4
Can recurrent diverticulitis be predicted?
Lucia Sobrinoa, Marta Climent, Clara Santanach, Sebastiano Biondo
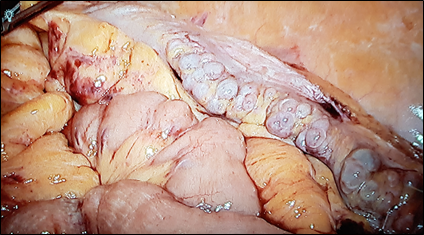
Diverticular disease is a common disorder, and recent guidelines report on new treatment strategies such as non-antibiotic management. Patients with diverticular disease are increasingly being treated as outpatients. In addition, fewer patients are undergoing emergency surgery whereas there is an increase in the use of elective and laparoscopic surgery in the management of diverticulitis. However, several aspects are still controversial. Strong evidence still lacks for the therapeutic management of patients with recurrent episodes of acute diverticulitis or patients with persistent abdominal symptoms after acute attacks. The European Society of Coloproctology (ESCP) guideline committee reviewed the literature and developed the European guidelines for the management of diverticular disease of the colon in 2020. In spite of the existence of several different classifications for diverticulitis, the committee decided neither to create another classification nor to endorse any of the existing ones. Nevertheless, phlegmonous diverticulitis, considered as uncomplicated by most of the classifications, is a matter of concern since it includes about 70% of the patients with acute diverticulitis. This group of patients may be clinically heterogeneous in terms of characteristics or disease evolution, which in some cases might be complicated. Patients at risk that belong to initially uncomplicated stage need to be identified in order to prevent complications and receive the most appropriate medical/surgical treatment. Classically, colonic resection after the second episode of acute diverticulitis has been supported, since any following episodes will respond insufficiently to medical treatment and with higher morbidity and mortality2. Recently, it was reported that 6.8-27.7%3,4 of patients with acute diverticulitis treated conservatively may require surgical intervention due to complicated diverticulitis or persistent symptoms, most of them during the first year of follow-up. In addition, elective sigmoidectomy seems to be related with a better quality of life (QOL) compared with conservative management in patients with recurring diverticulitis and/or ongoing complaints5,6. Nowadays, the main reason to perform elective sigmoid colectomy (Fig 1) in patients with recurrent disease or with ongoing symptoms after an acute episode of diverticulitis is to improve their QOL. In fact, there are many patients in whom initial antibiotic treatment fails, leading to sub-acute / chronic diverticulitis. In these patients the differentiation between sub-acute ongoing diverticulitis which never resolved, i.e. persisting disease, and a true recurrence is very difficult7. Chronic diverticulitis (Fig 1), considered as a true condition for the first time by the ESCP group, occurs when there is colonic wall thickening or chronic inflammation of the mucosa1. It can appear when an acute diverticulitis does not resolve completely, and it can have an important impact on QOL of the patients, causing persistent abdominal symptoms (abdominal pain, bloating) and changes in bowel habit. However, the uncertainty of the evolution of the disease and the lack of clear signs to identify which patients will develop a chronic condition, make the selection of patients and the best moment to advise surgical resection difficult. Colonic resection has been shown to effectively reduce the number of recurrences, but it should be kept in mind that it is a major surgery with potential severe complications1. The distinction between Irritable Bowel Syndrome (IBS) and symptoms related to chronic diverticulitis after an episode of diverticulitis is of utmost importance, because IBS is a functional disorder and should not be treated surgically8. Endoscopy could help in those cases where differential diagnosis is difficult5. It should be noted that after sigmoidectomy, 25% of patients persist with functional symptoms and abdominal pain9.
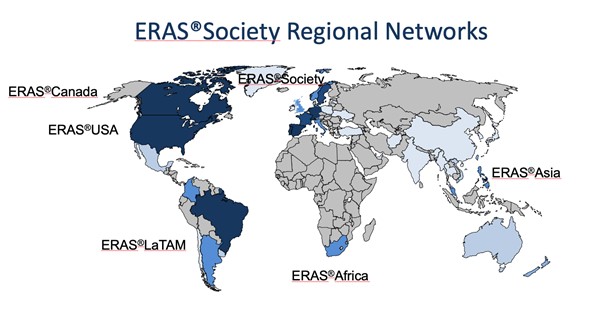
ERAS – yesterday, today and also for tomorrow? The ERAS Society perspective.
Olle Ljungqvist, Ulf Gustafsson, Hans D. de Boer
ERAS so far It is more than 25 years ago that a multimodal approach to recovery after major surgery, called fast track surgery, was first proposed1,2. Combined with laparoscopic surgery it showed that old and frail patients were fit to leave the hospital in two days after major surgery3. Larger follow up studies reported that this could be achieved with fast track surgery alone. This inspired a group of surgeons from Northern Europe to form the Enhanced Recovery After Surgery (ERAS) Study Group in 20014. The members hypothesized that bringing together all potential stress reducing and recovery improving care elements into one program, would enhance recovery after surgery. The first ERAS protocol was published in 20055. But alongside the guideline there was a need to also organize care in a new way to make ERAS fully functioning6 (Table 1). When the guideline was tested a clear relationship was shown with more care elements in the protocol in use and improved outcomes regarding both complications, length of stay and readmissions suggesting that detailed audit would be key7-9.
Copied!
