BJS Academy>Cutting edge blog>Oesophageal cancer a...
Oesophageal cancer awareness month 2025
Matthew Lee PhD FRCS
BHP Clinician Scientist & Honorary Consultant Colorectal Surgeon, University of Birmingham & University Hospitals Birmingham
5 February 2025
Guest blog Upper GI
Related articles

The future of obesity treatment
Pichamol Jirapinyo, MD, MPH, DABOM, FASGE, FACG
The International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) has released a consensus position statement addressing the integration of obesity management medications (OMMs) with metabolic bariatric surgery (MBS)1.
Currently, obesity treatment encompasses four primary modalities: lifestyle modification, OMMs, endoscopic bariatric and metabolic therapies (EBMTs), and MBS. The recent introduction of newer-generation OMMs, such as semaglutide and tirzepatide, has sparked a surge in their use and increased awareness of obesity as a treatable chronic disease2,3. While these medications show significant promise, they also have limitations, including non-response rates, potential adverse events, and challenges with long-term adherence.
This position statement is particularly timely, as an increasing number of patients who have tried or discontinued OMMs are now seeking additional interventions to support their weight management or maintenance goals. Furthermore, since not all patients respond optimally to MBS, incorporating adjunctive therapies, such as adding OMMs after surgery, should enhance outcomes.

Rethinking obesity treatment: a path towards sustainability and scalability
Robin P Blackstone, MD
Obesity, one of the most profound challenges of modern medicine, casts a shadow over global health, defying decades of simplistic advice to "eat less, move more." For decades, Metabolic and Bariatric Surgery (MBS) has transformed lives by altering the body’s interaction with food through metabolic mechanisms. For patients with severe obesity, surgery has delivered life-altering results, improved metabolic health and reframing obesity as a systemic disease. Yet, MBS is an inherently resource-intensive endeavour. From single-use instruments contributing to hospital waste to individualized preoperative requirements such as psychological evaluation and mandated weight-loss trials, surgery is costly and fundamentally unscalable. It is not a population-wide solution.
Pharmacological innovation offers a transformative opportunity to address this crisis. GLP-1 receptor agonists, with over a decade of real-world use, have redefined treatment possibilities. Medications like Liraglutide and Semaglutide rival the efficacy of surgery, delivering substantial weight loss and metabolic improvement without the invasiveness of an operation. Emerging therapies, such as Tirzepatide and a growing wave of oral agents, promise even greater precision and adaptability. These treatments are inherently scalable, with the potential to reach millions at a fraction of the cost of surgery. In some regions, these therapies are already available for less than $100 per month, opening the door to equitable, population-wide access.
The challenge now lies in navigating a thoughtful transition. MBS has undeniably saved lives, advanced our understanding of obesity, and reshaped public perceptions of its causes. But as pharmacotherapy evolves, the role of surgery will narrow, focusing on rare and complex cases—such as extreme obesity or anatomical complications—where medication alone may not suffice. This shift will demand the reimagination of surgical training, the adaptation of healthcare systems, and a commitment to equity in distributing life-saving medications.
Multimodal prehabilitation: beyond physical preparation
Fernando Dana
Major digestive surgery not only carries clinical risks but also imposes a significant functional and emotional burden. In this context, prehabilitation emerges as a key strategy to optimize patient readiness before entering the operating room.
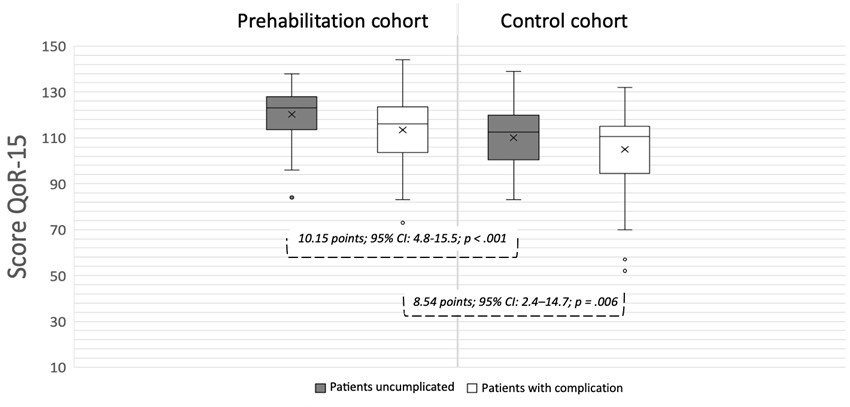
This analysis is based on a prospective cohort study conducted at a tertiary hospital, including 188 patients undergoing major elective gastrointestinal surgery. Of these, 94 completed a multimodal prehabilitation program, while 94 received standard preoperative care (Table 1). Outcomes were assessed using the validated QoR-15 questionnaire at baseline, discharge, and 30 days post-discharge, alongside clinical and functional recovery indicators (Figure 1).
Preoperative clinic data and type of surgery by group
Copied!
Connect

Copyright © 2026 River Valley Technologies Limited. All rights reserved.



.png)





.jpg)



